As critical care and emergency physicians on the front lines of the COVID-19 pandemic we were saddened and frustrated to read of the recent court order requiring Mercy Hospital in Coon Rapids to keep a patient on life support after it appears medical teams had determined that continued treatment would not benefit the patient ("Judge: COVID patient must be kept on ventilator," Jan. 15).
Since the advent of critical care in the 1950s, cases have been common in which a patient has no chance of survival despite best efforts, and essentially is dead but for the machines and interventions that keep the patient in medical purgatory, awaiting an infection, stroke or other event that yields final closure. This can take weeks, months or even years, but the outcome is a foregone conclusion.
The U.S. is nearly unique in allowing families and courts to intervene in these situations, and to order that artificial life support must continue. During times when adequate resources are available, these circumstances pose difficult financial and ethical considerations. When resources are scarce, the community consequences of continued active treatment become more significant and urgent — because other community members' lives are often at stake.
Today, as for the past several months, hundreds of patients are waiting in emergency departments in Minnesota for beds that are not available due to sustained and severe demands on hospitals. Some of these patients are critically ill or injured; they need trained personnel, a critical care unit, ventilators, dialysis machines, specialized treatments and diagnostics to prevent complications and death. Unfortunately, many of these patients never get a critical care bed. Many nonetheless recover, but some get worse and some die.
The average stay in intensive care, whether for a severe infection, a heart problem, trauma or other emergency condition is three days. Even during the 30 days the judge ordered Mercy to continue to provide artificial support (the patient has since been transferred to a Texas hospital), the intensive care resources involved could have benefited an additional 10 patients needing help.
It is never easy for families and care providers when a care team arrives at the decision that a patient cannot be benefited by further active treatment. Multiple opinions are sought, every angle is considered. The decision could not be more important, and it is treated that way.
Currently, it is estimated that 5 to 10% of all of our Minnesota critical care beds are occupied by patients receiving non-beneficial care at their families' request. Given the severity of illness and limited resources across the region, there are often no places to send them, so we continue to support them, expending precious resources, and experiencing the anguish of declining request after request from outside hospitals with other patients who need and could benefit from our services.
This is not to say that we are lowering our threshold for stopping active treatment due to scarce resources, but that the current scarcity sharply defines the trade-offs in devoting limited resources to a patient who cannot benefit.
Our resources are finite. Our citizens are suffering. Our hospital resources belong to the community and should not be used by individuals indefinitely to the detriment of others. The tragedy of the commons is real and we are compromising patient care today for many in our community by providing care that does not offer benefit.
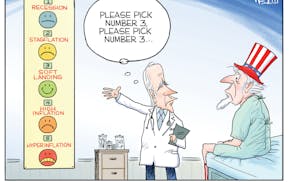
We urgently need to establish a national consensus and change the U.S. culture and expectations surrounding what treatments are provided at the end of life.
Health care teams are dedicated to serving our community; we spend years training and working to promote healing, relieve suffering, and help others survive and live as well as possible. We understand and share the desire to live, and the often excruciating challenge of making difficult treatment decisions as chances of survival fade and death approaches.
But there will be for each of us a point when death is coming. And often, when dying is not accepted, heroism becomes torture and harm is caused at every level, from patient to family to care team to community.
We do not know the specific details related to the case at Mercy Hospital; but we know our colleagues, and we know the very common circumstances faced in intensive care in all hospitals. We, your health care teams, are distressed, and these situations amplify that distress. Our workforce is exhausted and is contracting. We need your help.
For now, the best tool we have is to increase our vaccination and booster rates. With a fivefold reduction in illness and a 13-fold reduction in death, vaccinations clearly reduce demands for hospital care. Multiply this one case by the thousands of unvaccinated patients who dominate the demand for critical care in Minnesota, and we could have prevented unnecessary deaths and provided lifesaving care to countless others.
Please get vaccinated. Please consider what it means to be part of our community. We will do our best to care for you and continue to figure out the ethical boundaries where technology meets death.
John Hick, Michele LeClaire and Heidi Erickson are emergency and critical care physicians at Hennepin County Medical Center. The opinions expressed here are theirs alone and should not be interpreted as an official statement or position of Hennepin Healthcare.